On March 4th, 2024, I completed my 3rd round of chemo and was sent home from the hospital. I was walking without a cane and feeling pretty good. During the first week of recovery at home, I had the typical post-chemo side effects such as exhaustion, mild nausea, and the moderate emotional/psychological feelings of steroid withdrawal. [Pro-tip, ask your doctor to taper the dose of steroid so you don’t experience the withdrawal effects as much.] It was great to have regular visitors drop by my home. I also started to re-involve myself in normal household activities, like cooking and cleaning. My body weight was stabilizing which helped with my low blood pressure. I also was able to stop wearing my heated clothing 24/7.
My taste buds were quite sensitive, and I could no longer drink my home tap water. So I started buying spring water in large glass bottles. Unfortunately these were quite expensive but it was the only water I could tolerate. I was drinking 3 liters per day, and I quickly realized I could not afford to buy these bottles much longer. So, during one of my daily IV infusions, I researched various home water filtration systems. I settled on getting a reverse osmosis system that would run to our kitchen sink and refrigerator. This water tasted amazing and I’m so glad I made the investment.
Just as my body was moving into the 2nd phase of recovery, I started having radiating pain in my glute and down my leg. I forgot what it was like to have bad pain! It came on fast and was brutal. I had a hard time walking, sitting, and turning over in bed, and I couldn’t find a position to get relief. I immediately notified my oncologist through the online portal in case he felt it was something worth examining. He didn’t seem too concerned which was good news.
The next day, as my wife was hooking me up for my daily fluids, she noticed tiny red bumps in my arm. We both suspected blood clots. The bumps were small, but painful to the touch. There were three bumps in a line, along a vein in my forearm. My oncologist asked me to come down for visit, and unfortunately on a Friday, with peak Philadelphia traffic.
Luckily, I didn’t have to go to the ER and was seen by the NP in my oncologist’s office. She examined me and determined that my glute and leg pain was from sciatica, most likely aggravated by the many weeks of lying in bed. Having zero muscle or fat on my butt and not being very active, didn’t help much. The NP suggested I work with my physical therapist to try to alleviate the pain.
The bumps on my arm however, were more of an unknown. I had 2 NPs examine the bumps and they seemed to be stumped. And as they were examining me, I discovered several more bumps on the same arm. They were small, firm, painful and my skin was red at the sites. The NPs determined that I had swollen lymph nodes in my arm, and that seemed to be logical since I did have Lymphoma. Blood clots didn’t seem likely because of the size, location and amount of bumps I had. Yet, I wasn’t 100% sure these were from lymphatic tissue.
The next day was Saturday, March 16th. My son was participating in his first Karate tournament and I decided to attend. This was my first public outing in 3.5 months. It was a bit chilly outside but the sun felt warm and there was no wind. As we walked towards the auditorium, I was a little nervous about being in a crowd of people. Also, I was a bit self conscious about my appearance: still incredibly skinny, pale and obviously ill.
I walked into the auditorium and was shocked at the amount of people packed into the space, and especially the number of children. All that I could think about was the high quantities of bacteria and virus floating around in the room. Having a heavy duty N95 mask on my face only added to my self consciousness. I imagined people thinking, “Who is the guy wearing the mask? COVID is like so 3 years ago. This isn’t Whole Foods.”
Of course the tournament was running behind schedule and my son’s events were pushed back hours. I didn’t want to stay in the germ cesspool, so I sat outside in the sun (on my memory-foam cushion of course) and enjoyed the scenery. It was great to just sit and stare at the trees and sky without anything else to do. When it was time for my son’s events, I raced into the auditorium to watch him perform. It was really a special moment: I was so proud of him competing in karate; I was overjoyed to once again participate in his life activities and have him know I was there; and I was just excited to be alive.
Wednesday, March 20th I went back to HUP for round 4. First up was my ‘mid-chemo’ PET scan. I had completed 3 of the 6 rounds of the R-EPOCH chemotherapy regimen and it was time to see how my cancer was responding. Obviously things were moving in the right direction, but now we would see it on the screen. I arrived at HUP early in the morning for my scan. I received an injection of a radioactive glucose analog, and then waited an hour for that to travel around my body. Finally I got the scan, which took around 10 minutes. They said it would take a few hours to get the results and my doctor would review them with me. Of course I was quite anxious about getting the results. Many people including friends with cancer experience, and my nurses, predicted the results would be good due to the fact I was clinically improving so much. Recall that my first PET scan–during the first round of chemo– “lit up” with lymphoma everywhere. I had stage 4, meaning it had spread above and below my diaphragm, and in my bone marrow.
Finally it was time to meet with my oncologist. We sat waiting for a short while, until another young doctor came in to talk with us. He reviewed the result of the PET scan and stated there was no cancer detected! I asked about the detection of single cancerous cells, and he said the PET scan doesn’t have that type of resolution and that’s why they wanted to complete the full 6-cycle regimen. There would be three more rounds of chemo to presumably kill every last lymphoma cell. In summary, my PET scan results were the best outcome one could get. I will never forget March 20, 2024. My next PET scan would be after completing round 6, sometime in June.
With that good news, my oncologist entered the room and said, “We are upping your chemo dose by 20%.” I was worried about increased side effects but the doctor said I would probably not notice much difference. We also discussed the pros and cons of having my PEG tube (a plastic tube that goes from exterior abdomen into the stomach) removed during this round. I was torn between keeping it in case I become too nauseous to eat during rounds 4-6, versus not having to deal with a tube sticking out of my abdomen. I hadn’t used the tube for several weeks, other than 3x daily flushes to keep it clean. Yet, after weighing the pros and cons, my doctor advised to have it removed and I agreed.
The last thing we discussed during my visit was the tiny bumps in my arm. I had more now and my wife was adamant they were not swollen lymph nodes. My oncologist agreed the bumps were unusual so he scheduled an ultrasound to be performed after checking into the hospital that day.
After the consultation I was free to venture over to the hospital to get checked-in and start the initial process: COVID/Flu/RSV swab test, blood draw, admission questionnaire, liability releases, and so on.
My dilemma: no matter how early I got admitted and how much I tried to expedite the admission process, the chemo infusion didn’t start until very late at night. There were always delays and more delays due to their less-than-optimized process.
This round, for instance, I had to get an ultrasound on my arm before I was tied up the the chemo for 5 days. It turns out my wife was right, and I had blood clots all over my arm. This was the arm where my PICC line was located. The clots could have been the result of the very first (two) IV lines that were put in my arm at the small local hospital back in January. Or they could be the result of me not really using that arm much because of the PICC line limiting arm movement. Since the clots were on my arm and palpable, they were not a major concern, as opposed to deep vein clots in the legs which can be deadly. The doctor prescribed a daily low-dose aspirin in addition to the daily blood thinner injection I always received while in the hospital.
After all the delays, my chemo finally got going around midnight, again! I don’t like starting chemo late at night because the IV bag runs for 24 hours, which means the nurses would need to hook up a new bag at around 1 am the next night. But there were always delays and the bag switch would creep each night: 1 am, 2 am, 3 am. There were so many other nightly interruptions in the hospital and it really disrupted sleep. But the biggest sleep disruptor was the periodic beeping of the IV pump. This was either caused by lots of tiny air bubbles in the line (they call EPOCH the “champagne chemo”), or a kink in the line from my arm being in a bad position. The beeping could happen as much as every hour to 30 minutes. Once the pump starts beeping, I was supposed to call the nurse, but by this round I started to fix the machine myself (don’t tell anyone).
First drug up is rituximab. Rituximab is a monoclonal antibody against the protein CD20, mostly found on the surface of B cells (both normal and cancerous). When the antibody binds to CD20 it triggers cell death. Rituximab can have immediate side effects, typically an allergic reaction, so they give “pre-meds” such as Benadryl (and Tylenol, I assume to just make you feel better). Since I could swallow pills now, I just took Benadryl capsules as opposed to IV Benadryl. [Let me tell you, IV Benadryl is brutal. I got that during Round Two and I thought I was going to die from it.] Once the rituximab started, the nurse checked vitals several times to make sure there were no problems. After about an hour or so, the rituximab was done and they could hook me up to the main chemo bag, kicking off the 5 day treatment.
I was concerned about the increased dose, however the side effects were pretty similar to the previous round: slight nausea, loss of appetite, and lethargy. All manageable.
The next day I had my lumbar puncture (LP) where they drain fluid for pathology and also inject methotrexate as a preventative– in case there are any lymphoma cells in my spine/brain. The regular chemo doesn’t cross the blood/brain barrier. I really didn’t like LPs but I knew it was very necessary.
The following day I had my PEG tube removed. The interventional radiology nurse came to my room and said she would just pull it out right there. I asked if it would hurt and she said, “yes, it will be painful but the pain won’t last long.” I appreciated the honesty and I could prepare for the pain. She ripped it out in a half-second. Indeed, it hurt but after about 5 minutes I felt much better.[Note the pain ratio of getting the PEG surgically placed into my stomach vs the quick removal was around 100:1.] The nurse said I would likely have a “bullet hole” scar on my abdomen, which in the scheme of things is no big concern to me.
During this 4th round I was able to move around much better. I took walks around the entire floor, at least once per day. The entire floor-loop is 1/4 mile. I also tried to walk around the room as much as possible. I read that getting a lot of water and exercise helps with the chemo side effects. My sister visited again this round so she would encourage me to move around and she walked the halls with me.
I’m always admitted to one of two oncology floors at the hospital, so I knew that every patient I saw had cancer. It was really sad to see so many others with cancer and I wonder if they thought the same thing about me. I know when I walked the halls, I clearly looked like a cancer patient — bone skinny, pale, no hair, slight limp, and dragging an IV pole.
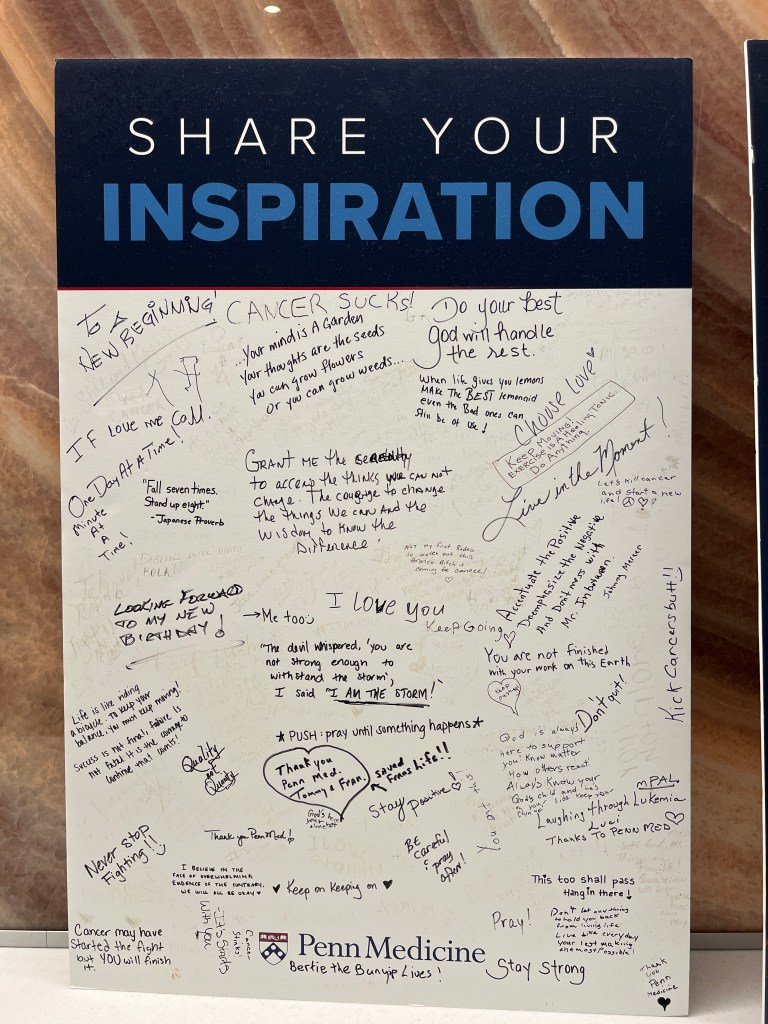
On one walk, I went to the lounge area with a nice view of downtown Philly. In the lounge were two large foam-core board signs. One was about cancer survivors and the other featured inspirational messages written by patients and visitors. The one message that stuck with me was “Your mind is a garden, your thoughts are seeds. You can grow flowers or you can grow weeds.”
I had a new outlook on life, that’s for sure.
On the morning of March 25th, my wife and son arrived to pick me up and I was waiting for them with my bags packed. I had packed up my entire room myself and was eager to get home.
Take away: Think flowers.
_________________________________
Continue reading ‘Part 9:’ https://vincepaton.com/2024/03/15/cancer-journey-part-9-chemo-rounds-five-and-six-final-round/
————————————————
Get notifications when a new post is published. Subscribe here: https://vincepaton.com/about/
