Burkitt’s lymphoma is a highly treatable cancer, with a promising remission/cure rate (when caught early enough), however it is also the most aggressive cancer.
Before I get into the details, I’ll give you a quick summary of my background. I have a master’s degree in molecular biology and have published several research papers while working in academia. Near the start of my career, I worked in a lab studying mechanisms of prostate cancer prevention. This work really shaped my adult life and my determination to attempt to prevent cancer as best I could. In my current career outside of research, I work with pharma companies and have to know a bit about cancer drugs, as well as be fluent in discussing the inter-workings of clinical trials- especially for cancer drugs. So I know a fair amount about cancer. I know it well enough to fear it and hoped I could avoid it through disciplined lifestyle choices. Yet, in all these years, I never studied much about lymphomas and the wide spectrum of lymphoma subtypes. What I’ve recently learned specifically about Burkitt’s lymphoma, a rare Non-Hodgkin lymphoma subtype, makes me really appreciate where I am right now compared to just a couple of months ago. It also makes me realize some things are just back luck.
When my symptoms first started, cancer was not on my radar. It obviously wasn’t on anyone else’s either. The probability of getting cancer is pretty low, and with my health record and lifestyle habits, it didn’t seem too likely at my age. When I received the results of my first blood test, cancer was my first thought. I was still hopeful I had something else like an infection or a rheumatological disease, as was suggested by several doctors I had seen. But indeed, it turned out to be lymphoma.
It wasn’t until after my 4th round of chemotherapy that I had the time and the emotional space to finally sit down and learn about my new diagnosis of Burkitt’s lymphoma. At the time of diagnosis I didn’t receive the “Burkitt’s Lymphoma and You” brochure (which doesn’t exist), and I was not in any physical state to read something about the horror I was going through. In this blog post, I intend to share some of the information I’ve recently discovered on Burkitt’s lymphoma and lymphoma in general.
But before getting into the details, here are some cancer basics:
What exactly is cancer? Cancer occurs when cells in the body start dividing uncontrollably. There are two main types of cancers: solid and blood. Solid tumors, which form masses, can be benign (non-cancerous) or malignant (cancer that can spread throughout the body). Blood/liquid cancers, like leukemias and lymphomas, affect the blood and lymph systems respectively and therefore spread throughout the body easily.
For the sake of my story, I’m going to briefly describe leukemia and lymphoma before focusing on Burkitt’s.
Leukemia originates in the bone marrow and results in the high production of abnormal white blood cells. These cells circulate in the bloodstream and can affect the bone marrow’s ability to produce other types of blood cells. Leukemia cells usually spread throughout the body, potentially affecting various organs and interfering with the normal function of blood cells, leading to issues like anemia, infection, and bleeding disorders. In fact, when I was first admitted to the Hospital of the University of Pennsylvania, they thought I had some type of leukemia based on a few initial test results.
Lymphoma, however, specifically affects the lymphatic system. It leads to the formation of cancerous lymphocytes, which are a type of white blood cell. These abnormal cells often form tumors in lymph nodes and other parts of the lymphatic system. Lymphoma tends to remain more localized to lymphatic tissue (like lymph nodes, spleen, and thymus) but can spread to other organs over time, including bone marrow. After only a few hours at HUP, the doctors were able to determine that I actually had a form of lymphoma. The odd thing was, I had no visible or palpable swollen lymph nodes. I had no masses. My cancer had been completely hidden from typical detection.
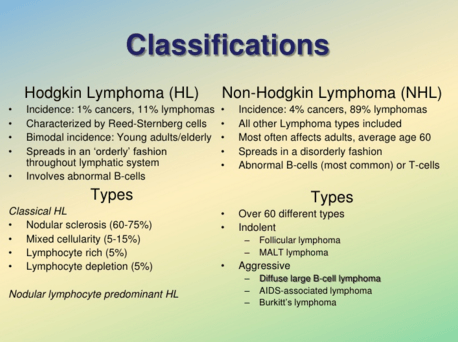
Lymphoma has two primary types: Hodgkin lymphoma (HL) and Non-Hodgkin lymphoma (NHL).
I won’t go into HL much, but will just say that these cancers are more treatable and have higher success rates than compared to the many NHL subtypes.
NHL encompasses a diverse group of subtypes that vary greatly in their severity, progression, and prognosis. The variability in NHL subtypes makes overall treatment and prognosis more complicated compared to Hodgkin lymphoma. Subtypes range from indolent (slow) to highly aggressive forms. Burkitt’s lymphoma is a highly aggressive form of NHL, but on the more treatable end of the spectrum due to its responsiveness to chemotherapy. Other NHL’s are slow-growing and not curable but manageable as chronic diseases. The effectiveness of treatment can depend significantly on the stage at diagnosis, the specific type, and individual patient factors such as age and overall health.
Burkitt’s lymphoma, known for being highly aggressive, is treatable, especially when diagnosed early. The definition of “early” in this context is before the disease has spread to the central nervous system (CNS), or has compromised vital organs. Also treatment is more effective if certain symptoms are not present such as night sweats, high fevers, and rapid weight loss. When diagnosed, I had symptoms of all of those above. The doctors at HUP initially suspected the lymphoma had infiltrated my CNS due to the neuropathy I was experiencing. However, after 2 negative lumbar punctures, it was determined that the lymphoma was not in my CNS. This was excellent news.
Burkitt’s lymphoma grows very quickly, which means it can spread to the central nervous system and vital organs rapidly, making this disease go from stage 1 to stage 4 in just weeks. This rapid growth requires swift and intensive treatment which is hard to do with a healthcare system that often takes weeks if not months to navigate. My journey to diagnosis took about 6 weeks from symptom onset. I was stage 4 by then. (See Cancer Journey Part 1, Cancer Journey Part 2 and Cancer Journey Part 3)

Despite Burkitt’s aggressiveness, it responds well to intensive chemotherapy, which can often lead to high cure rates. I consider this a double-edged sword. Without treatment, Burkitt’s is rapidly fatal. But because the lymphoma cells grow so much faster than any other normal cells in the body, they are highly vulnerable to chemotherapy and can be wiped out just as quickly. Thus the success rates can be as high as 80%. Note that some normal cells do grow faster than others, such as hair follicles which are highly susceptible to chemotherapy. My hair did fall out after round one as is typical with most chemotherapy treatments.
I have read so many times that Burkitt’s is “aggressive.” This is obvious to me based on my personal experience, but what does that mean with respect to other cancers? I have been doing some digging to satisfy my own curiosity, but also I feel the need to explain to others–including doctors–just how aggressive Burkitt’s is.
What I’ve recently learned is that breast cancer, for example, has a median cell doubling time of 100 days. Meaning the amount of cancer cells double in approximately 100 days (of course there are many types of breast cancers and they vary in their aggressiveness). Burkitt’s has a median doubling time of 36 hours or 1.5 days. So with each 1.5 days of Burkitt’s left untreated, it is similar to 66 days of untreated breast cancer. Other cancers that are considered highly aggressive like small cell lung cancer (SCLC) and certain aggressive forms of pancreatic cancer also have relatively short doubling times. The doubling time for SCLC, for example, can be around 30 days. This is still 20x slower than Burkitt’s. I try to explain this to people so they understand that the seemingly short delay in my diagnosis of about 20 days, was like delaying a breast cancer diagnosis by 3.6 years. Would you want that? I wish doctors could have understood this. That is partly the reason behind this entire blog. I am hoping that my experience can possibly help others understand the urgency to diagnose and treat aggressive cancers.
The cause of Burkitt’s lymphoma is partly known. I say partly, because no one can every really know why one person gets cancer and another doesn’t. Part of it is simply bad luck. There is thought to be 3 different causes or types of Burkitt’s, but all 3 involve an error in the DNA of an immature B cell. The malfunction in the B cell can be initiated by either (1) Epstein-Barr virus, (2) HIV, or (3) a spontaneous, random error during the cell’s DNA replication (which can be the cell’s own error or an error caused by external forces such as radiation or harmful chemical exposure). Burkitt’s does not involve an inherited mutation like many other cancers and diseases. This means the DNA mutation isn’t passed down from a parent, and a victim of Burkitt’s cannot pass it down to future children. The error happens in B cells and not in sperm or egg. This was one of the first questions I had after my diagnosis. I have a 7 year old son so one of my first thoughts was, “Will I pass this down to him?”
The treatment regimen for Burkitt’s lymphoma typically involves more aggressive chemotherapy protocols than many other lymphomas. These regimens can be highly effective but also come with a significant risk of side effects.
I’ve been receiving the R-EPOCH regime and thus far the side effects have been tolerable. (See Appendix A below for a background on R-EPOCH.) For further reading, here is a good overview of Burkitt’s and various treatment protocols. https://lymphoma.org/understanding-lymphoma/aboutlymphoma/nhl/burkitt/
How do we know R-EPOCH is working? Well, I’m walking, talking, eating and feeling pretty normal again. That’s proof enough for my doc and a win for me. I’m getting better and the cancer has stopped doubling.
One thing I have learned from my wife’s experience with two chronic illnesses and a recent breast tumor (that was thankfully benign), and now my own lymphoma, is to seek out the best doctor right away if time allows. Even something as seemingly standard as a biopsy can be radically different between doctors or facilities. My bone marrow biopsy which was done at a small local hospital “wasn’t a good one” according to my current oncologist. The pathology study wasn’t totally definitive between Burkitt’s and Diffuse Large B Cell lymphoma, another NHL. These two subtypes of NHL can be hard to differentiate. If my bone marrow biopsy was performed at HUP where I am now being treated, I’m certain the sample would have been a good one and determined the NHL subtype with certainty and undergone DNA sequencing to reveal any and all underlying mutations. Nonetheless, the team at HUP made a nuanced decision to diagnose me with Burkitt’s based on pathology and clinical symptoms and my progress makes us all feel that right decision was made.
The pathology report did however include information on the specific genetic translocation (a chunk of DNA was erroneously moved to another chromosome) for my lymphoma. It is the most common one for Burkitt’s but also can happen in DLBCL (there’s the nuance and possible confusion between the two NHL’s). This translocation helps explain why Burkitt’s is so aggressive: in simple terms, there’s a gene called Myc that controls how often a cell will replicate. In my translocation, the Myc gene was moved to a spot just in front of a gene “promoter” (ie the “on/off switch” for a gene) that is always turned on (in this case the gene promoter was the immunoglobulin heavy gene, IgH). So this combination creates a “photocopy machine gone haywire” with copies of Myc shooting out nonstop. Since the Myc protein tells the cell to divide as fast as possible, the cell and all of its progeny (offspring) are cancerous. Burkitt’s lymphoma cells divide about every 24-36 hours, which is the fastest growth of any cancer. When my wife said that I was ‘dying in front of her’ she wasn’t being dramatic.
As mentioned previously, the ultra-fast growth of Burkitt’s lymphoma cells makes them particularly susceptible to chemotherapy. Drugs work best on targets that are distinguishable from healthy cells. For instance, bacteria differ significantly from human cells, allowing antibiotics to target and eliminate them without much harm to our bodies. Similarly, the fast-replicating lymphoma cells in Burkitt’s demand substantial nutrients so they quickly drink up anything around them, including chemo drugs. Chemotherapy exploits their hungry appetite to disrupt the lymphoma cell replication, ultimately causing the cells to die. Other cells, not growing as rapidly, are less affected because they’re not rapidly drinking the chemotherapy drugs.
One of the agents in the R-EPOCH regimen operates differently from traditional chemotherapy. The ‘R’ in R-EPOCH stands for rituximab, a monoclonal antibody that specifically targets B cells. It attaches to the surface of these cells, marking them for destruction by the immune system, irrespective of whether they are cancerous (so it quite weakens the immune system). Post-chemotherapy, a special growth factor shot—costing $4,000 per dose from Pfizer!—is administered to stimulate the production of new B cells, safeguarding against serious infections due to depleted B cell levels. Thankfully, my insurance covers most of this cost, leaving me with a manageable co-insurance payment.
While R-EPOCH is quite effective, it naturally comes with side effects. Life is about trade-offs, and in this case, the benefits of chemotherapy vastly outweigh the risks. The alternative—untreated Burkitt’s lymphoma—is a guaranteed death. Common side effects of the treatment are generally tolerable, although there are more severe potential complications, including the possibility of developing another cancer from traditional chemotherapy components like EPOCH. However, in facing such a dire prognosis, one must focus on the immediate threat, “playing the hand that’s in front of them” without dwelling excessively on less probable future risks, many of which are beyond our control.
On a lighter note: How rare is Burkitt’s lymphoma? There are about 1200 new cases diagnosed in the US each year. By comparison there are over 330,000 new US cases of breast cancer diagnosed each year. I assume that the underlying mutation as described above is a very rare event thus making the disease quite uncommon. I will probably be the only person you will ever know with Burkitt’s and if you don’t know me, you will probably never hear of this disease from anyone else. Also as mentioned earlier, the genetic cause of Burkitt’s is not inherited from parents. It is a spontaneous event that comes from either external exposure (such as radiation or chemicals, or certain viruses) or from an accidental error in the cell’s DNA replication machinery. There’s not much one can do about the latter and it is just bad luck. My lymphoma was most likely caused by a random event and not due to a virus, but either way, it’s bad luck.
Take away: Do not delay getting medical attention.
Appendix A: R-EPOCH, Technical Overview
The chemotherapy regimen known as R-EPOCH was developed to improve outcomes in patients with aggressive non-Hodgkin lymphomas, including diffuse large B-cell lymphoma (DLBCL). Here’s a brief overview of its development:
Background and Origin: EPOCH stands for Etoposide, Prednisone, Oncovin (vincristine), Cyclophosphamide, and Hydroxydaunorubicin (doxorubicin). The regimen was originally developed in the 1990s by the National Cancer Institute (NCI) as a dose-adjusted strategy to optimize the dosing based on patient tolerance and response. The aim was to maximize the efficacy of the drugs while minimizing toxicity. Introduction of Rituximab: Rituximab is a monoclonal antibody that targets the CD20 protein found on the surface of B-cells, making it effective against diseases that involve these cells, such as many types of non-Hodgkin lymphoma. The addition of rituximab (indicated by the “R” in R-EPOCH) to the EPOCH regimen was based on its success in improving outcomes in other lymphoma treatments.
Rationale and Development: The rationale behind the development of R-EPOCH was based on the concept of infusional chemotherapy, where drugs are given continuously over several days rather than in quick doses. This approach maintains a constant drug concentration in the bloodstream, potentially increasing the treatment’s efficacy and reducing side effects.
Clinical Trials and Adoption: Early clinical trials showed that R-EPOCH was effective in patients with poor prognostic features who had aggressive lymphomas. Over time, studies confirmed that adding rituximab to the regimen improved the overall survival rates and reduced the risk of disease progression.
Current Usage: Today, R-EPOCH is used extensively for treating aggressive B-cell lymphomas and is considered a standard treatment for certain cases, particularly for patients with high-risk disease features. The development of R-EPOCH is a good example of how treatment regimens evolve through clinical research and the integration of new therapeutic agents, aiming to provide more effective and personalized cancer care.
————————————————
Get notifications when a new post is published. Subscribe here: https://vincepaton.com/about/

Thank you, Vince…..from a fellow traveller. I have added a link to your blog, to a couple of other Fb Lymphoma support groups. Hope you don’t mind.
Alan Smith, Brisbane, Australia.
LikeLike
Thank you, Vince….from a fellow traveller. I finished my six months of R-EPOCH in October 2022…and so far, so good!!
LikeLike
My son,20 yr, had stage 4 in 2020 and was at HUP. Drs Barta, Chong were fantastic. He’s good now!
Think HUP would share this w new patients? Have your docs read this? It is so beautifully written.
Back then I was given a thick handout on RA-EPOCH. At dx. Path report talked about MYC, CD20, etc. Thanks to you, now I finally know what MYC does.
Thank you for thinking about other Burkitt survivors and families. Writing this has to have been tough while recovering. Thank you so much, Vince!
LikeLike
Thank you for reading and thank you for the compliment.
LikeLike